Steroids, Treatments, Potency, Types of Steroids, Side Effects, OTC Brand Generics
Table of Contents
Corticosteroids
What Are Corticosteroids
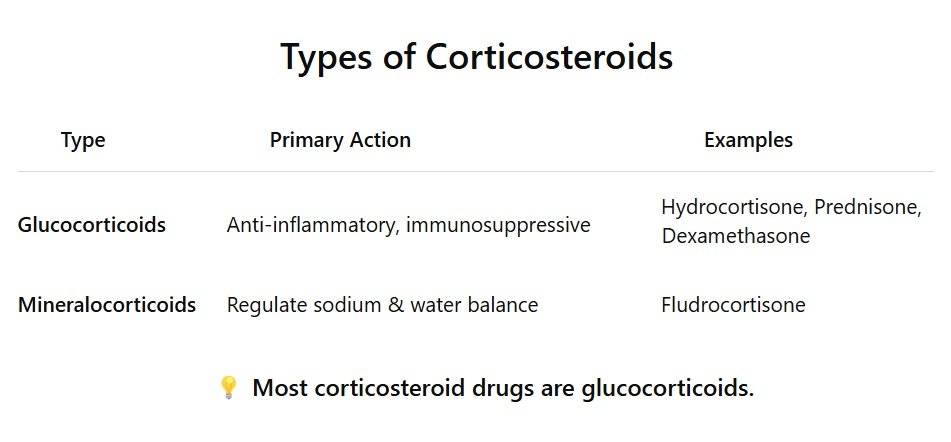
Corticosteroids are man-made drugs that mimic hormones your body naturally produces in the adrenal cortex (the outer part of the adrenal glands above your kidneys). Corticosteroids are often known as steroids.There are two main types:
Glucocorticoids
Glucocorticoids control inflammation, immune response, and metabolism.Example: Prednisone, Dexamethasone
Mineralocorticoids
Mineralocorticoids control salt and water balance in the body.Example: Fludrocortisone
How Steroids Work
Basic Mechanism of Action:
- Corticosteroids enter your cells (they’re lipid-soluble, so they pass through cell membranes easily).
- Inside the cell, they bind to glucocorticoid receptors in the cytoplasm.
- This drug-receptor complex moves into the nucleus of the cell.
- Once in the nucleus, it turns certain genes on or off, especially those that:
- Suppress inflammation
- Inhibit immune system responses
- Reduce the production of inflammatory substances like prostaglandins, cytokines, and leukotrienes
Basically, corticosteroids tell the body to calm down the inflammation and immune overreaction.
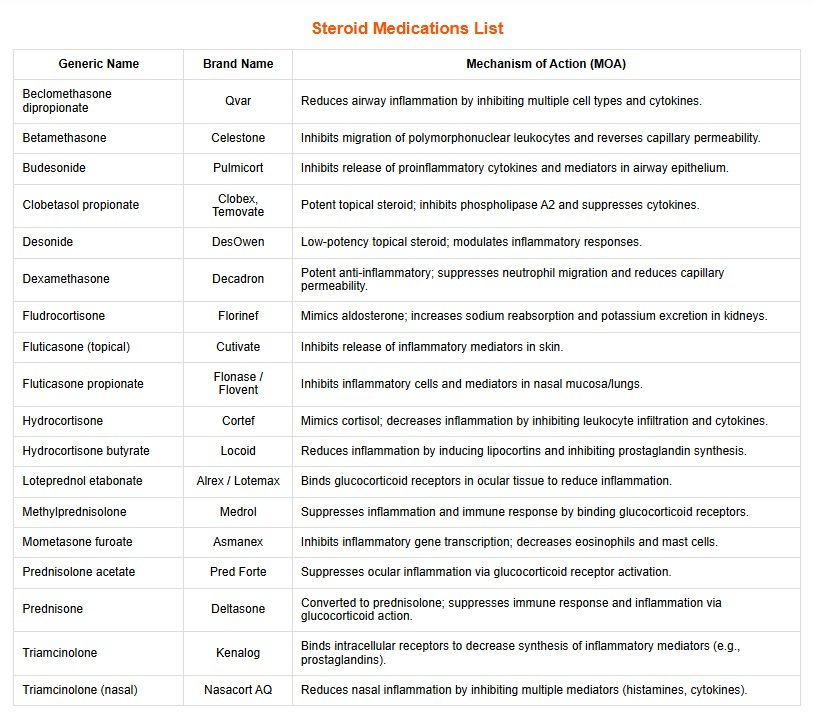
Steroid Medications List
| Generic Name | Brand Name | Mechanism of Action (MOA) |
| Beclomethasone dipropionate | Qvar |
Reduces airway inflammation by inhibiting multiple cell types and cytokines.
|
| Betamethasone | Celestone |
Inhibits migration of polymorphonuclear leukocytes and reverses capillary permeability.
|
| Budesonide | Pulmicort |
Inhibits release of proinflammatory cytokines and mediators in airway epithelium.
|
| Clobetasol propionate | Clobex, Temovate |
Potent topical steroid; inhibits phospholipase A2 and suppresses cytokines.
|
| Desonide | DesOwen | Low-potency topical steroid; modulates inflammatory responses. |
| Dexamethasone | Decadron |
Potent anti-inflammatory; suppresses neutrophil migration and reduces capillary permeability.
|
| Fludrocortisone | Florinef |
Mimics aldosterone; increases sodium reabsorption and potassium excretion in kidneys.
|
| Fluticasone (topical) | Cutivate | Inhibits release of inflammatory mediators in skin. |
| Fluticasone propionate | Flonase / Flovent | Inhibits inflammatory cells and mediators in nasal mucosa/lungs. |
| Hydrocortisone | Cortef |
Mimics cortisol; decreases inflammation by inhibiting leukocyte infiltration and cytokines.
|
| Hydrocortisone butyrate | Locoid |
Reduces inflammation by inducing lipocortins and inhibiting prostaglandin synthesis.
|
| Loteprednol etabonate | Alrex / Lotemax | Binds glucocorticoid receptors in ocular tissue to reduce inflammation. |
| Methylprednisolone | Medrol |
Suppresses inflammation and immune response by binding glucocorticoid receptors.
|
| Mometasone furoate | Asmanex |
Inhibits inflammatory gene transcription; decreases eosinophils and mast cells.
|
| Prednisolone acetate | Pred Forte | Suppresses ocular inflammation via glucocorticoid receptor activation. |
| Prednisone | Deltasone |
Converted to prednisolone; suppresses immune response and inflammation via glucocorticoid action.
|
| Triamcinolone | Kenalog |
Binds intracellular receptors to decrease synthesis of inflammatory mediators (e.g., prostaglandins).
|
| Triamcinolone (nasal) | Nasacort AQ |
Reduces nasal inflammation by inhibiting multiple mediators (histamines, cytokines).
|
Forms of Steroids
- Topical – creams, ointments, lotions
- Oral – tablets, capsules, solutions
- Inhaled – asthma and COPD
- Nasal sprays – allergies
- Injectable (IM/IV) – severe allergic reactions, inflammation
- Rectal – for ulcerative colitis
- Ophthalmic – eye drops
What Steroids Treat
- Asthma & COPD
- Allergic reactions
- Autoimmune diseases (e.g., lupus, RA)
- Skin conditions (eczema, psoriasis)
- Inflammatory bowel disease (Crohn’s, UC)
- Adrenal insufficiency (Addison’s)
- Certain cancers
- COVID-19 (severe cases)
Side Effects of Steroids
Short-Term Use:
- Insomnia
- Weight gain
- Mood changes
- Increased appetite
- High blood sugar
- Water retention
Long-Term Use:
- Skin thinning
- Osteoporosis
- Muscle wasting
- Immune suppression
- Cataracts/glaucoma
- Adrenal suppression
- “Cushingoid” appearance (moon face, buffalo hump)
Adverse Effects of Steroids
Topical Steroids
- Skin atrophy, striae, telangiectasia
- Hypopigmentation (especially in darker skin)
- Perioral dermatitis (with prolonged facial use)
Systemic Steroids
- Metabolic: Hyperglycemia, weight gain, moon face
- Musculoskeletal: Osteoporosis, myopathy
- Immunosuppression: Increased infection risk
- Endocrine: HPA axis suppression, Cushing’s syndrome
Steroids important points to Remember
- Tapering: Don’t stop high-dose or long-term steroids suddenly — risk of adrenal crisis!
- Take with food: Reduces stomach irritation.
- Monitor blood sugar in diabetics.
- Inhaled steroids can cause oral thrush — rinse mouth after use.
- Topical steroids: Use lowest strength needed for shortest duration.
Steroids Potency Chart (Topical & Systemic)
| Generic Name | Generic Name | Brand Name | Dosage Form Available |
|
Class 1 – Super Potent
|
Betamethasone dipropionate (augmented) 0.05% | Diprolene, Diprolene AF | Cream, Ointment, Gel, Lotion |
| Clobetasol propionate 0.05% | Temovate, Clobex, Olux, Cormax, Embeline | Cream, Ointment, Gel, Foam, Lotion, Shampoo | |
| Diflorasone diacetate 0.05% | Psorcon, Apexicon E | Cream, Ointment | |
| Fluocinonide 0.05% | Lidex | Cream, Ointment, Gel, Solution | |
| Fluocinonide 0.1% | Lidex-E | Cream | |
|
Class 2 – Potent
|
Amcinonide 0.1% | Cyclocort (Canada), generic | Cream, Ointment, Lotion |
| Betamethasone dipropionate (augmented) 0.05% | Diprolene AF | Cream (Augmented), Lotion | |
| Desoximetasone 0.25% | Topicort | Cream, Gel | |
| Diflorasone diacetate 0.05% (non-augmented) | Maxiflor, generic | Cream, Ointment | |
| Fluocinolone acetonide 0.2% | Synalar HP | Cream | |
| Halcinonide 0.1% | Halog | Cream, Ointment, Solution | |
| Halobetasol propionate 0.05% | Ultravate, Bryhali | Cream, Lotion | |
|
Class 3 – Upper Mid-Strength
|
Amcinonide 0.1% | Cyclocort (Canada), generic | Cream, Lotion |
| Betamethasone valerate 0.1% (ointment) | Luxiq, generic | Ointment | |
| Desoximetasone 0.05% | Topicort LP | Cream, Ointment | |
| Fluocinolone acetonide 0.025%–0.2% | Synalar | Cream, Solution, Ointment | |
| Fluticasone propionate 0.005% (ointment) | Cutivate | Ointment | |
| Halometasone 0.05% | Halovate (not widely available in U.S.) | Cream, Ointment | |
| Mometasone furoate 0.1% (ointment) | Elocon | Ointment | |
| Triamcinolone acetonide 0.5% | Aristocort A, Kenalog | Cream, Ointment | |
|
Class 4 – Mid-Strength
|
Clocortolone pivalate 0.1% | Cloderm | Cream |
| Fluocinolone acetonide 0.025% | Synalar | Cream, Solution, Ointment | |
| Flurandrenolide 0.05% | Cordran | Cream, Ointment, Tape | |
| Hydrocortisone valerate 0.2% | Westcort | Cream, Ointment | |
| Mometasone furoate 0.1% (cream/lotion) | Elocon | Cream, Lotion | |
| Triamcinolone acetonide 0.1% | Kenalog, Aristocort A | Cream, Ointment | |
|
Class 5 – Lower Mid-Strength
|
Desonide 0.05% | DesOwen, Tridesilon, Verdeso | Cream, Lotion, Gel, Ointment |
| Fluocinolone acetonide 0.01% | Derma-Smoothe/FS, Fluonid | Oil (used for the scalp) | |
| Fluticasone propionate 0.05% | Cutivate | Cream, Lotion | |
| Hydrocortisone butyrate 0.1% | Locoid | Cream, Ointment, Lotion | |
| Mometasone furoate 0.1% (cream) | Elocon | Cream | |
|
Class 6 – Mild
|
Alclometasone dipropionate 0.05% | Aclovate | Cream, Ointment |
| Desonide 0.05% | DesOwen, Tridesilon, Verdeso | Cream, Lotion, Gel, Ointment | |
| Fluocinolone acetonide 0.01% | Derma-Smoothe/FS | Oil (used for the scalp) | |
| Hydrocortisone butyrate 0.1% | Locoid | Cream, Ointment, Lotion | |
|
Class 7 – Least Potent (Often OTC)
|
Fluocinolone acetonide 0.01% | Derma-Smoothe/FS | Oil (scalp) |
| Hydrocortisone 1% | Cortizone-10, Aveeno HC, Hydrocortisone 1%, Preparation H | Cream, Ointment, Lotion, Gel, Spray | |
| Hydrocortisone 2.5% | Generic, Cortaid 2.5% | Cream, Ointment, Lotion | |
| Hydrocortisone acetate 1% | Hytone | Cream, Ointment | |
| Hydrocortisone butyrate 0.1% | Locoid | Cream, Ointment |
Steroids Potency Chart Important Notes:
Corticosteroids, especially topical ones are often classified by potency, which refers to how strong their anti-inflammatory effects are on the skin or tissues.Here’s how they’re divided by potency, particularly for topical corticosteroids (creams, ointments, lotions):
There are 7 classes in the U.S., with Class 1 being the most potent and Class 7 the least potent.
- Augmented formulations (e.g., Diprolene) enhance skin penetration, increasing potency.
- Potency can vary between cream, ointment, lotion, or gel forms, even with the same drug.
- Even the same steroid can be stronger or weaker depending on its form:
- Ointments > Creams > Lotions
- Ointments are more occlusive and penetrate better, making them more potent.
- Use lower-potency steroids for thin-skinned areas (face, groin, axillae, infants).
What skin conditions are treated with steroids?
Corticosteroids are primarily used to reduce inflammation and suppress the immune response in various skin conditions, but they are generally not used as the first-line treatment for infected skin. However, they can be prescribed in certain cases when there is an underlying inflammatory skin disorder that coexists with a mild infection or when secondary infections complicate conditions like eczema or psoriasis.Here’s a breakdown of skin infections and inflammatory conditions that may be treated with corticosteroids:
Inflammatory Skin Conditions with Secondary Infections. Corticosteroids may be prescribed for skin conditions that have an inflammatory component, which also have a risk of secondary bacterial or fungal infections.
Eczema (Atopic Dermatitis)
- Corticosteroids are often used to treat inflammation and itching in eczema.
- Secondary bacterial infections like Staphylococcus aureus (common in eczema) can complicate eczema.
- Corticosteroids help manage the eczema but are often combined with antibiotics when there is a secondary infection.
Psoriasis
- Corticosteroids are used to treat the inflammatory symptoms of psoriasis, and topical corticosteroids can help reduce scaling, redness, and itching.
- Psoriasis is associated with secondary fungal or bacterial infections due to broken skin or excessive scratching.
Contact Dermatitis
- If a contact dermatitis rash becomes infected (e.g., from scratching or bacterial contamination), corticosteroids may help reduce inflammation.
- Topical antibiotics may be needed if a secondary infection is present.
Seborrheic Dermatitis
- Corticosteroids can be used to control inflammation in seborrheic dermatitis, which may occur with fungal infections like Malassezia.
- If there is a fungal component, antifungal treatment may also be needed alongside corticosteroids.
Acne with Inflammation
- In cases of inflamed acne, topical corticosteroids may reduce redness, swelling, and irritation. However, steroid acne (a specific type of acne caused by corticosteroid use) can develop if corticosteroids are used excessively or improperly.
- Oral corticosteroids are sometimes used in severe acne (e.g., cystic acne) to reduce inflammation.
Steroids use as combination therapy
Corticosteroids are often used as combination therapy with antifungals or antibacterial medications for treating skin conditions that involve both inflammation and infection. The goal is to manage the inflammatory symptoms (such as swelling, redness, and itching) while also addressing the underlying fungal or bacterial infection.Here are some common skin conditions where corticosteroids are combined with antifungal or antibacterial treatments:
Fungal Infections with Inflammation
These conditions involve fungal infections that require both antifungal agents and corticosteroids to control inflammation and itching.Tinea (Ringworm)
- Tinea infections (e.g., tinea corporis, tinea cruris, tinea pedis, tinea capitis) are fungal infections that often require antifungal medications like clotrimazole, miconazole, or terbinafine.
- If the infection is causing severe inflammation, topical corticosteroids (e.g., hydrocortisone, betamethasone) may be added to reduce swelling, redness, and itching.
- However, corticosteroids should be used cautiously, as they can sometimes worsen fungal infections or cause them to spread.
Candidiasis (Yeast Infection)
- Candidiasis (caused by Candida species) can affect areas like the skin folds, groin, or oral cavity.
- When Candida infections cause significant inflammation, a combination of antifungal medications (e.g., fluconazole, clotrimazole) and topical corticosteroids (e.g., hydrocortisone) may be used.
- Corticosteroids help alleviate itching and redness while the antifungal targets the yeast infection.
Seborrheic Dermatitis with Fungal Component
- Seborrheic dermatitis is a chronic inflammatory condition often associated with the fungus Malassezia.
- Combination therapy includes topical antifungals (e.g., ketoconazole, ciclopirox) to treat the fungal infection, along with corticosteroids (e.g., fluocinolone, mometasone) to reduce inflammation, scaling, and itching.
- This combination is commonly used for scalp or facial seborrheic dermatitis.
Bacterial Infections with Inflammation
In some cases, bacterial infections can cause significant inflammation, and corticosteroids may be used alongside antibiotics to reduce the inflammatory response.Impetigo
- Impetigo is a superficial bacterial skin infection often caused by Staphylococcus aureus or Streptococcus pyogenes.
- Topical antibiotics like mupirocin or retapamulin are used to treat the infection, and corticosteroids (e.g., hydrocortisone) may be added to reduce inflammation, swelling, and itching.
- Corticosteroids are typically used only after the infection has started to resolve, to avoid worsening the infection.
Eczema with Secondary Bacterial Infections
- Atopic dermatitis (eczema) is often complicated by secondary bacterial infections, particularly Staphylococcus aureus.
- Topical corticosteroids (e.g., fluticasone, betamethasone) are used to reduce the inflammation of eczema.
- When a secondary bacterial infection is present, topical antibiotics (e.g., mupirocin) or oral antibiotics (e.g., cephalexin) are used in conjunction with corticosteroids to treat both the infection and inflammation.
Folliculitis
- Folliculitis is an infection of the hair follicles that can be caused by bacteria (usually Staphylococcus aureus).
- Antibiotics (topical or oral) such as mupirocin or clindamycin are used to treat the bacterial infection.
- Corticosteroids (e.g., hydrocortisone) may be used in combination to reduce inflammation, itching, and swelling.
Dermatitis with Secondary Fungal or Bacterial Infections
Certain types of dermatitis can lead to secondary infections, and combination therapy may include both antibiotics or antifungals and corticosteroids.Contact Dermatitis with Secondary Infection
- Contact dermatitis (from irritants or allergens) can become infected with bacteria or fungi.
- Corticosteroids like hydrocortisone or betamethasone are used to control the inflammation of contact dermatitis.
- If a secondary bacterial infection is present, antibiotics (e.g., mupirocin) are used.
- If the dermatitis is complicated by fungal infection, an antifungal agent (e.g., ketoconazole) may be used in addition to the corticosteroid.
Lichen Planus with Secondary Infections
- Lichen planus is a chronic inflammatory condition that can affect the skin, nails, and mucous membranes. In some cases, it may become infected, especially with bacteria or fungus.
- Corticosteroids (e.g., clobetasol, fluocinonide) are used to reduce the inflammation of lichen planus.
- Antifungal or antibiotic therapy may be needed if there is a secondary infection.
Steroids Use Precautions in Skin Infections
- Corticosteroids should not be used in active untreated fungal or bacterial infections because they can suppress the immune response and worsen the infection.
- Topical corticosteroids may be used cautiously in some situations but must be combined with appropriate antimicrobial therapy (antibiotics or antifungals).
- Infection management always takes precedence, and corticosteroids should only be used for inflammatory control once the infection is under control.
- Antifungal or antibacterial treatment should always be addressed first and may be combined with corticosteroids once the infection is under control.
- Combination therapy helps to manage both the infection and inflammation, but the infection itself should always be the primary concern.