Indications of medications and dietary supplements
OTC Medications vs. Prescription Medications: Laws and Regulations
Over-The-Counter Meds (OTC)
- Over-the-Counter (OTC) Medications: Drugs that can be sold directly to consumers without a prescription.
- OTC Drugs: Must meet FDA-established safety and effectiveness standards for use without medical supervision.
- OTC Medications: Must include Drug Facts Label with active ingredients, usage, warnings, and dosage.
- These can be sold in pharmacies, supermarkets, and online
- May provide advice but no prescription needed
- Controlled Substances are not included
Prescription Meds
- Prescription Medications: Require a Patient Package Insert (PPI) or Medication Guide for safety information.
- Prescription Drugs: Require a doctor’s evaluation due to potential risks, side effects, or misuse concerns.
- Prescription Medications: Drugs that require a healthcare provider’s authorization before being dispensed.
- These are only available at pharmacies with a prescription
- prescription medications must be verified before dispensing
- Regulated by provider’s prescription and federal laws
- Controlled substances are included as a part of prescription medications
Switching from Prescription to OTC (Rx-to-OTC Switch)
Some medications become OTC after the FDA determines they are safe for self-use (e.g., omeprazole for acid reflux, loratadine for allergies).What are different schedules of drugs
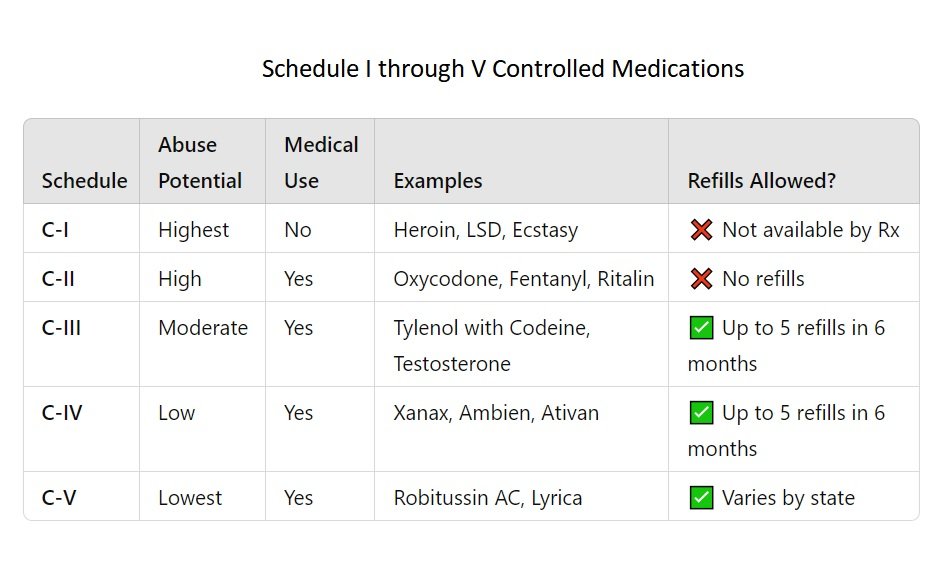
Schedule I (C-I)
Schedule i drugs have currently no accepted medical use and come with a high potential for abuse. Examples:- Heroin
- LSD (lysergic acid diethylamide)
- Ecstasy (MDMA)
- Marijuana (federally, although legal in many states)
- Cannot be prescribed or dispensed.
- Only used in research under strict conditions.
- Have highest potential for abuse with no medical use.
Schedule II (C-II)
Schedule ii drugs have significant acceptable medical use but a high potential for abuse, which may lead to severe physical or psychological dependence. Examples:- Oxycodone (OxyContin, Percocet)
- Morphine
- Fentanyl
- Methamphetamine
- Methylphenidate (Ritalin, Concerta)
- No refills allowed.
- A new prescription is required for each fill.
- Often limited to a 30-day supply.
- Electronic prescribing (EPCS) is often required.
- Have high potential for abuse.
Schedule III (C-III)
Schedule-iii drugs have moderate to low potential for physical and psychological dependence.
Examples:
- Tylenol with Codeine (acetaminophen/codeine)
- Buprenorphine (Suboxone)
- Anabolic steroids (e.g., testosterone)
Rules:
- Prescription valid for 6 months.
- Up to 5 refills allowed within that 6-month period.
Schedule IV (C-iv)
Schedule-iv drugs have low potential for abuse and risk of dependence.
Examples:
- Alprazolam (Xanax)
- Diazepam (Valium)
- Lorazepam (Ativan)
- Zolpidem (Ambien)
Rules:
- Same as Schedule III: valid for 6 months, up to 5 refills.
- Often prescribed for anxiety, sleep disorders, or seizures.
Schedule V (C-V)
Schedule v drugs have the lowest potential for abuse, often used for antidiarrheal, antitussive, or analgesic purposes.
Examples:
- Cough syrups with <200 mg codeine per 100 mL (e.g., Robitussin AC)
- Lomotil (diphenoxylate/atropine)
- Pregabalin (Lyrica)
Rules:
- Prescription or OTC depending on the state.
- Some states in US sell schedule 5 drugs in limited quantities without a prescription. (Please check individual state laws).
Patient Package Insert (PPI), vs Medication Guide (MG) vs Instructions for Use (IFU)
What is a Patient Package Insert (PPI)?
A Patient Package Insert (PPI) is a leaflet or document included with certain prescription medications that provides the patient with detailed information about the drug. It is written in consumer-friendly language and is designed to help patients understand how to safely and effectively use the medication.
PPIs are regulated by the U.S. Food and Drug Administration (FDA) and are required for specific drug categories, particularly those with serious risks or complex administration instructions.
FDA Regulations for PPIs
According to FDA regulations (21 CFR 208), a Patient Package Insert must be:- Provided with every prescription fill, including refills.
- Dispensed by pharmacists in both retail and hospital settings.
- Written in non-technical, patient-friendly language.
- Updated regularly to reflect new safety information or changes in usage.
- Estrogens (e.g., conjugated estrogens like Premarin)
- Oral contraceptives (e.g., birth control pills)
Most Common Medications That Require Patient Package Inserts (PPIs)

Benefits of Patient Package Inserts (PPIs)
Improve Patient Understanding- PPIs explain what the drug is, how to take it, and what to watch for, empowering patients to make informed decisions.
- By outlining side effects, warnings, and interactions, PPIs help reduce medication errors and increase adherence.
- Dispensing a PPI can protect against legal claims of failure to warn about risks.
- Patients can better understand potential risks and benefits before taking the medication.
- Especially for drugs with Boxed Warnings, PPIs help reduce misuse or misunderstanding.
Patient Package Inserts (PPI) vs Medication Guides (MG) vs Instructions for Use (IFU)
Patient Package Inserts (PPI), Medication Guides (MG), and Instructions for Use (IFU) are three types of FDA-approved written materials that are provided to patients, ensuring safe and effective use of medications. They all have slight differences and some similarities.
Patient Package Insert (PPI)
A Patient Package Insert (PPI) is written information required by the FDA to be dispensed with specific prescription drugs, mainly oral contraceptives and estrogen-containing products.Purpose: To educate patients on the uses, risks, side effects, and proper use of certain medications.
When is it Required:
Federally mandated for:
- Estrogens
- Oral contraceptives
- What the drug is used for
- How to take it
- Risks and side effects
- Warnings and precautions
- Manufacturer’s contact info
Medication Guide (MG)
A Medication Guide is FDA-required labeling for medications that pose a serious and significant public health concern.Purpose: To inform patients of essential safety information, such as risks of severe side effects, misuse, or non-compliance.
When is it required: FDA requires a Medication Guide if:
- It could prevent serious adverse effects
- Patient decision-making depends on it
- Instructions for safe use are critical
- Opioids (risk of addiction/overdose)
- Isotretinoin (Accutane) (risk of birth defects)
- Warfarin (risk of bleeding)
- Antidepressants (risk of suicidal thoughts)
- Must be given with each fill (initial and refill)
- Pharmacists are responsible for dispensing it
Instructions for Use (IFU)
Instructions for Use (IFU) are FDA-required patient-directed instructions for complex medications or devices that require special handling or administration.Purpose: To guide patients through proper administration techniques for medications or devices to ensure correct and safe use.
When is it Required:
- For drugs with unique delivery methods
- When misuse could lead to harm or ineffective treatment
- Injectable medications (e.g., insulin pens, auto-injectors)
- Inhalers (e.g., asthma medications)
- Topicals or transdermal patches (e.g., testosterone gel)
- Eye drops or ear drops
- Intranasal sprays
- Step-by-step use instructions
- Diagrams or images
- Storage and disposal info
- What to do if a dose is missed
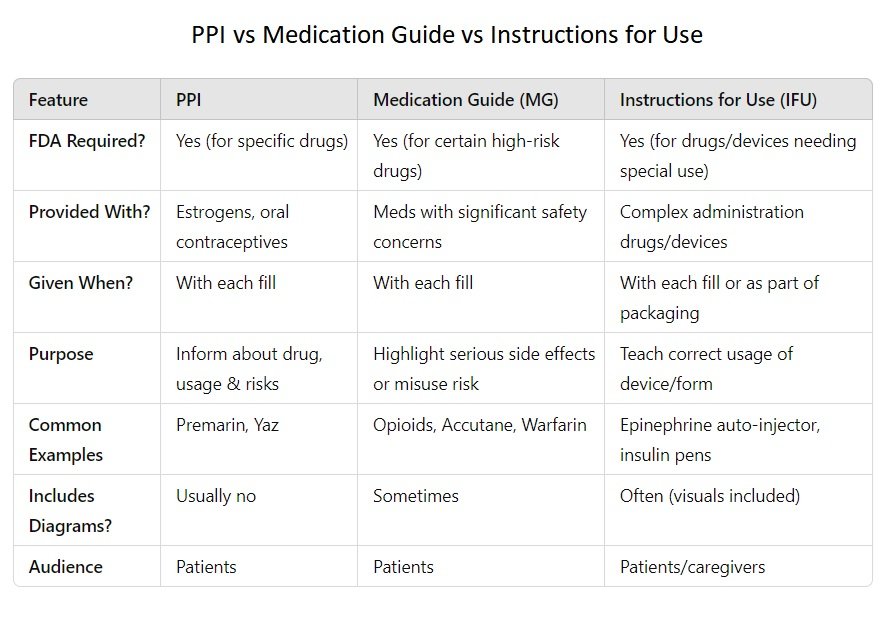
PPI = Basic patient information for estrogens/oral contraceptives
MG = Critical safety warnings for high-risk medications
IFU = Step-by-step guide for how to use a drug or device correctly
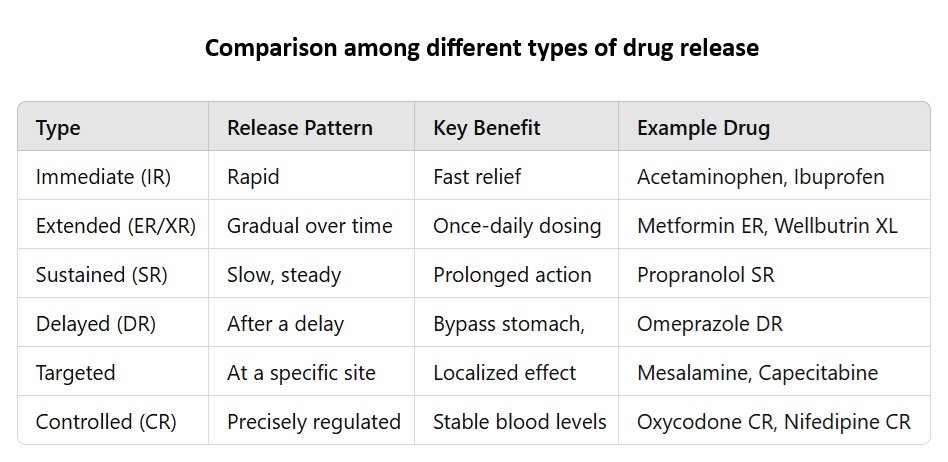
What is Drug Release?
Drug release refers to the process by which a drug is released from its dosage form (e.g., tablet, capsule, patch, or implant) and becomes available for absorption into the bloodstream. It is a critical factor in determining the drug’s therapeutic effectiveness, onset of action, duration of effect, and safety.Different Types of Drug Release Mechanisms
1. Immediate Release (IR)
How it works:
- The drug dissolves quickly after administration.
- Designed to disintegrate rapidly in the gastrointestinal (GI) tract.
- Absorption starts within minutes.
Benefits:
- Fast onset of action.
- Useful for acute conditions like pain or fever.
- Simple and cost-effective.
Examples:
- Acetaminophen (Tylenol IR)
- Ibuprofen (Advil)
- Diphenhydramine (Benadryl)
2. Extended Release (ER / XR / XL)
How it works:
- Releases the drug gradually over time.
- Maintains consistent drug levels in the blood.
- Often taken once daily.
Benefits:
- Less frequent dosing.
- Better patient compliance.
- Reduced risk of side effects from peak drug levels.
Examples:
- Metformin ER (Glucophage XR) – for diabetes.
- Bupropion XL (Wellbutrin XL) – for depression.
- Venlafaxine XR (Effexor XR) – for anxiety/depression.
3. Sustained Release (SR)
How it works:
- Releases drug slowly and steadily over an extended period.
- Maintains therapeutic levels for a longer time.
Benefits:
- Prolonged drug effect.
- Less fluctuation in plasma drug levels.
- Reduced dosing frequency.
Examples:
- Propranolol SR – for hypertension.
- Theophylline SR – for asthma/COPD.
- Diltiazem SR – for angina or high blood pressure.
4. Delayed Release (DR)
How it works:
- Drug release is intentionally delayed after ingestion.
- Often used to bypass stomach acid and release in intestines.
- Commonly uses enteric coating.
Benefits:
- Protects stomach from irritating drugs.
- Protects acid-sensitive drugs from stomach acid.
- Targeted release in specific areas of GI tract.
Examples:
- Omeprazole DR (Prilosec) – enteric-coated PPI.
- Aspirin DR (Ecotrin) – to prevent stomach irritation.
- Doxycycline DR (Doryx) – to improve GI tolerance.
5. Targeted Release
How it works:
- Delivers the drug to a specific site (e.g., colon, tumor).
- Often uses specialized coatings or drug carriers like nanoparticles.
Benefits:
- Higher efficacy at the target site.
- Minimizes systemic side effects.
- Useful in cancer, GI diseases, etc.
Examples:
- Mesalamine (Asacol HD, Pentasa) – targets colon in ulcerative colitis.
- Capecitabine (Xeloda) – prodrug activated in tumor cells.
- Liposome-encapsulated Doxorubicin – targets cancer cells.
6. Controlled Release (CR)
How it works:
- Precisely controls the rate and duration of drug release.
- More advanced than sustained release.
- Can combine multiple mechanisms for control.
Benefits:
- Maintains consistent therapeutic levels.
- Reduces dosing frequency and side effects.
- Improves patient adherence.
Examples:
- Oxycodone CR (OxyContin) – pain management.
- Nifedipine CR (Adalat CC) – for hypertension.
- Morphine CR (Kadian, MS Contin) – chronic pain relief.
What determines the choice of dosing in medications?
Nature of the Drug (Pharmacokinetics & Stability)
Half-life of the drug:
- Short half-life: May benefit from extended or controlled release to avoid frequent dosing. Example: Metformin ER (instead of multiple doses of IR).
- Long half-life: Often given as immediate release.
Drug solubility:
- Poorly soluble drugs might need special formulations to improve absorption (like delayed or controlled release).
Stability in the stomach:
- Acid-sensitive drugs may need delayed release (enteric coating). Example: Omeprazole (a proton pump inhibitor).
Desired Onset and Duration of Action
Rapid action needed? – Choose immediate release (IR).
Example: Acetaminophen IR for quick pain relief.
Long-term effect required? – Use extended/sustained/controlled release.
Example: Oxycodone CR for 12-hour pain control.
Site of Action in the Body
Local vs. systemic action:
- Local (e.g., colon, tumor) – Targeted or delayed release. Example: Mesalamine DR for ulcerative colitis (releases in colon).
- Systemic – IR, SR, ER depending on treatment goals.
Disease or Condition Being Treated
Chronic conditions (e.g., hypertension, diabetes):
- Benefit from extended or controlled release for once-daily dosing and stable drug levels.
Acute conditions (e.g., fever, pain, allergic reaction):
- Need immediate release for quick relief.
Patient Factors
Adherence (compliance):
- Extended/controlled release reduces pill burden (once daily vs. multiple times).
- Easier for elderly or patients with complex regimens.
Tolerance to side effects:
- Controlled or sustained release can reduce peak concentrations and side effects.
Swallowing difficulty:
- Some extended-release tablets can’t be crushed. Liquid or chewable IR forms may be needed.
Manufacturer’s Goals & Drug Delivery Technology
Innovation or patent extension:
- Companies may develop extended-release forms of older drugs to improve convenience or create new market advantages.
Technology available:
- Liposomes, nanoparticles, osmotic pumps, etc., may allow more advanced drug targeting or release control.
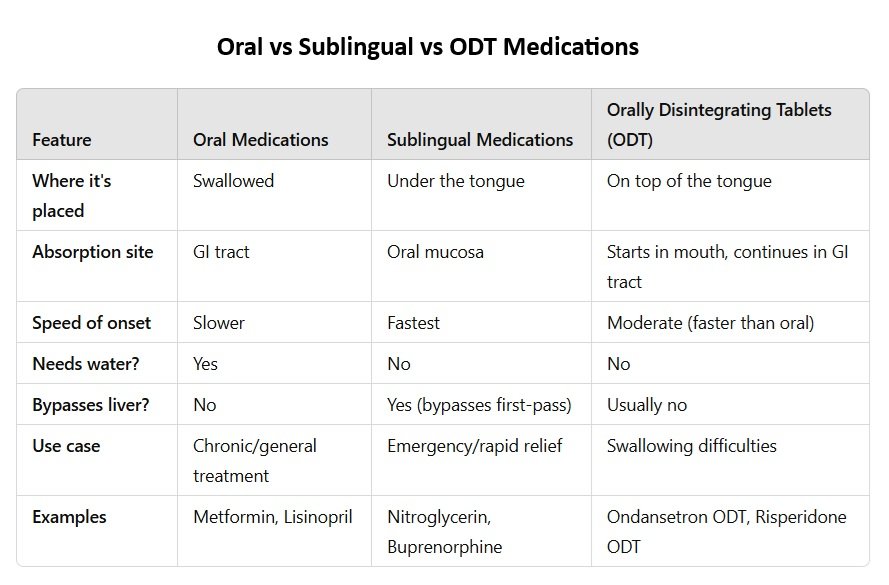
Oral Medications, Sublingual Medications and Orally Dissolving Tablets (ODT)
Let’s discuss the similarities and differences among oral medications, sublingual medications, and orally dissolving tablets (ODTs) based on route, absorption, speed, with examples.
Oral Medications (Swallowed)
- Route: Swallowed and absorbed through the gastrointestinal (GI) tract.
- Absorption site: Mostly in the small intestine.
- Onset of action: Slower (typically 30 minutes to 2 hours).
- First-pass metabolism: Yes (passes through the liver before entering circulation).
- Formulations: Tablets, capsules, syrups, solutions, etc.
- Use cases: Chronic conditions, general treatment.
Examples:
- Metformin tablets (for diabetes)
- Lisinopril (for high blood pressure)
- Acetaminophen (Tylenol tablets)
Sublingual Medications (Under the Tongue)
- Route: Placed under the tongue and absorbed directly into the bloodstream.
- Absorption site: Oral mucosa (rich in blood vessels).
- Onset of action: Very fast (1–5 minutes).
- First-pass metabolism: Bypassed — drug enters bloodstream directly.
- Formulations: Sublingual tablets, films, sprays.
- Use cases: Emergencies, drugs needing rapid effect.
Examples:
- Nitroglycerin SL tablets (for chest pain)
- Buprenorphine SL (opioid dependence)
- Zolpidem SL (Edluar) – for insomnia (rapid sleep induction)
Orally Disintegrating Tablets (ODT)
- Route: Placed on the tongue; dissolves quickly without water.
- Absorption site: Begins in the mouth, but mostly swallowed and absorbed in GI tract.
- Onset of action: Faster than regular oral tablets, but slower than sublingual.
- First-pass metabolism: Usually yes (if swallowed).
- Formulations: Fast-melt tablets, films.
- Use cases: Useful for patients with trouble swallowing (children, elderly, nausea).
Examples:
- Ondansetron ODT (Zofran) – for nausea.
- Risperidone ODT (Risperdal M-Tab) – for schizophrenia.
- Meloxicam ODT (Qmiiz) – for pain/inflammation.
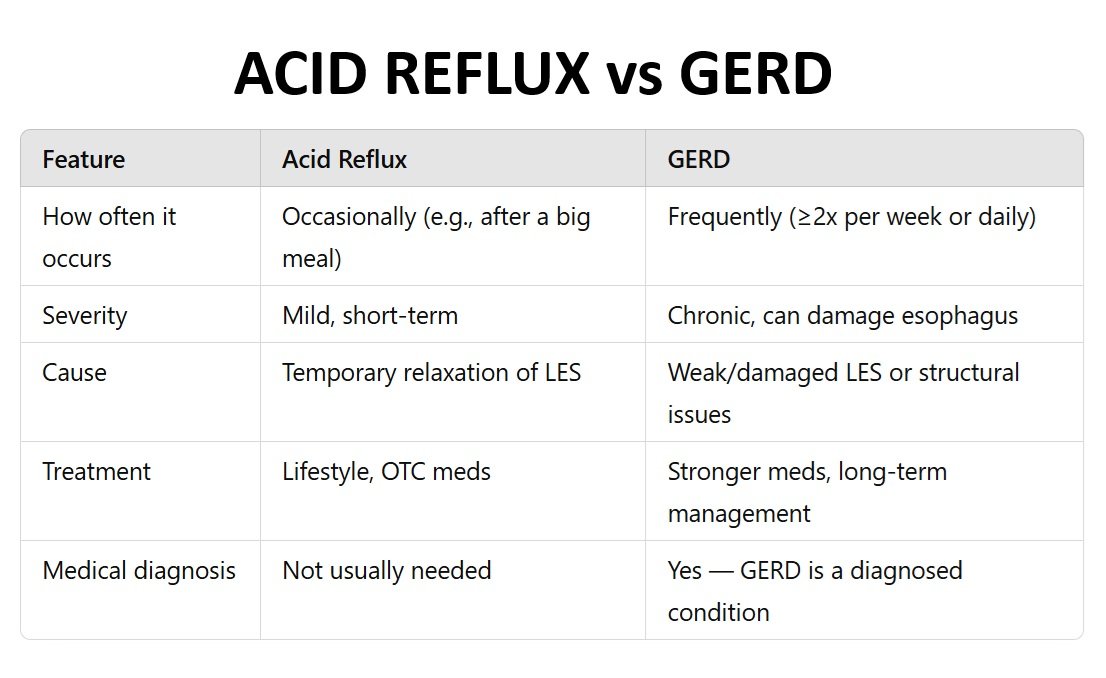
Acid REFLUX and GERD
What is Acid Reflux?
- Acid reflux is a condition where stomach acid flows backward into the esophagus, the tube connecting your mouth and stomach.
- This happens when the lower esophageal sphincter (LES), a ring-like muscle — doesn’t close properly after food enters the stomach.
- This causes heartburn, a burning sensation in the chest or throat.
Common Symptoms:
- Heartburn (burning sensation in the chest or throat)
- Sour or bitter taste in the mouth
- Regurgitation of food or acid
- Bloating or burping
What is GERD (Gastroesophageal Reflux Disease)?
- GERD is a chronic and more severe form of acid reflux.
- It’s diagnosed when acid reflux symptoms occur two or more times (2+) per week or cause complications.
- It’s considered a disease, not just a symptom.
- Over time, GERD can cause damage to the esophagus (like inflammation, ulcers, or narrowing).
- Esophagitis (inflammation of the esophagus)
- Difficulty swallowing
- Chronic cough or sore throat
- Chronic cough, hoarseness, sore throat
- Feeling of a lump in the throat
- Worsening asthma

Acid Reflux Treatment / Drug Classes
Antacids
Neutralize stomach acid (fast relief)
How they work:
- React with stomach acid to reduce acidity.
- Onset: Fast (minutes)
- Duration: Short (1–2 hours)
- Use: Occasional / temporary relief
Common Antacids:
- Calcium carbonate – Tums, Rolaids
- Magnesium hydroxide – Milk of Magnesia
- Aluminum hydroxide – Maalox
- Combo products – Gaviscon, Mylanta
Good for: Quick relief of occasional heartburn
Caution: May cause constipation (aluminum) or diarrhea (magnesium)
Proton Pump Inhibitors (PPIs)
Strongly block acid production (long-term control)
How they work:
- Inhibit proton pumps in stomach lining, reducing acid at the source.
- Onset: Slower (1–3 days for full effect)
- Duration: Long-lasting (24+ hours)
- Use: Chronic GERD, ulcers, erosive esophagitis
Common PPIs:
- Omeprazole – Prilosec
- Esomeprazole – Nexium
- Lansoprazole – Prevacid
- Pantoprazole – Protonix
Best for: Long-term control of GERD
Caution: Risk of vitamin B12 deficiency, osteoporosis, infections (C. diff) with long-term use
H2 Receptor Blockers (H2RAs)
Reduce acid production (medium relief)
How they work:
- Block histamine receptors in the stomach that trigger acid release.
- Onset: 30–60 minutes
- Duration: 6–12 hours
Common H2 Blockers:
- Ranitidine (withdrawn in many markets)
- Famotidine – Pepcid
- Cimetidine – Tagamet
Good for: Moderate, longer-lasting relief
Caution: Tolerance can build with long-term use
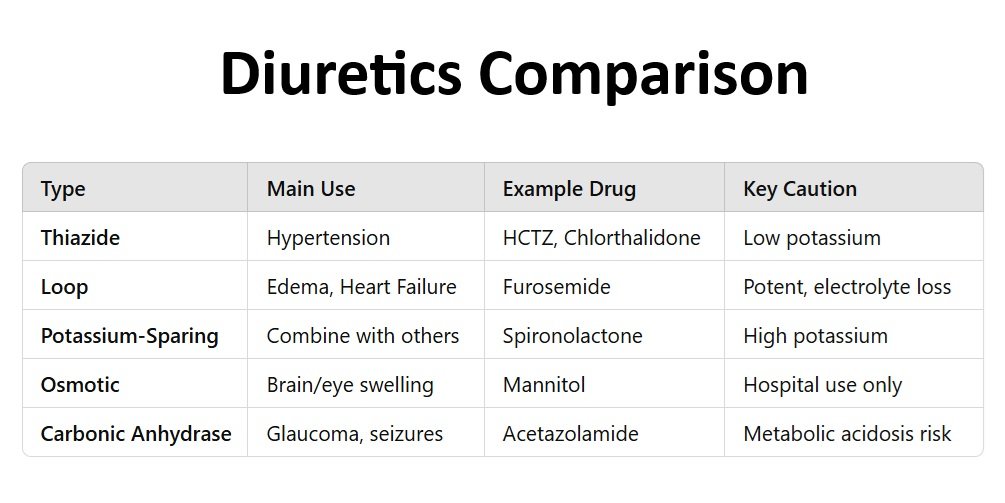
Diuretics
Why Are Diuretics Used?
Diuretics are used to treat conditions where the body holds on to too much fluid or where reducing blood pressure is needed.Common Conditions Treated:
- High blood pressure (hypertension)
- Heart failure
- Edema (swelling due to fluid buildup)
- Kidney disorders
- Liver cirrhosis
- Glaucoma (specific diuretics)
- Certain cases of hypercalcemia (high calcium)
Types of Diuretics
1. Thiazide Diuretics
- How they work: Act on the distal convoluted tubule in the kidney to reduce sodium reabsorption.
- Used for: High blood pressure, mild edema
- Hydrochlorothiazide (HCTZ)
- Chlorthalidone
- Indapamide
2. Loop Diuretics
- How they work: Act on the loop of Henle in the nephron, very powerful diuretics.
- Used for: Edema from heart failure, kidney disease, liver disease
- Furosemide (Lasix)
- Bumetanide
- Torsemide
3. Potassium-Sparing Diuretics
- How they work: Work in the collecting ducts, help retain potassium while removing sodium.
- Used for: Often combined with other diuretics to balance potassium loss
- Spironolactone (also treats hormonal acne, heart failure)
- Eplerenone
- Amiloride
- Triamterene
4. Carbonic Anhydrase Inhibitors
- How they work: Inhibit carbonic anhydrase enzyme; weak diuretics
- Used for: Glaucoma, altitude sickness, some seizure types
- Acetazolamide
5. Osmotic Diuretics
- How they work: Pull water into the urine by changing osmotic pressure
- Used for: Emergency reduction of intracranial or intraocular pressure
- Mannitol
What are Side Effects of Diuretics
- Dehydration
- Electrolyte imbalances (low potassium, sodium, magnesium)
- Frequent urination
- Dizziness or low blood pressure
- Gout (especially with thiazides)
- Increased blood sugar or cholesterol (some thiazides)
Diuretics vs Potassium: What’s the Connection?
Diuretics That Lower Potassium (Cause Hypokalemia)
These increase potassium loss in the urine.
Too much loss = hypokalemia (low blood potassium)
Examples:
- Thiazide diuretics
- Hydrochlorothiazide (HCTZ), Chlorthalidone
- Loop diuretics
- Furosemide (Lasix), Bumetanide, Torsemide
⚠️ Risks:
- Muscle weakness or cramps
- Irregular heartbeat
- Fatigue
- Dangerous if combined with other potassium-lowering meds (like digoxin)
Potassium-Sparing Diuretics (Help Retain Potassium)
These prevent potassium loss or increase potassium levels Can cause hyperkalemia (high blood potassium)Examples:
- Spironolactone
- Eplerenone
- Triamterene
- Amiloride
- High potassium (hyperkalemia)
- Irregular heartbeat
- Especially dangerous in kidney disease or when taken with ACE inhibitors or ARBs
What Are Contraceptives?
Contraceptives are methods or devices used to prevent pregnancy. They work by interfering with the normal process of ovulation, fertilization, or implantation of a fertilized egg.
Key Points:
- Also called birth control.
- Some methods are temporary (e.g., pills, condoms), while others are permanent (e.g., sterilization).
- Some contraceptives also offer protection against sexually transmitted infections (STIs), like condoms.
What Are Different Types of Contraceptives?
Categorization is based on how contraceptives work.What Are Different Types of Contraceptives?
Categorization is based on how contraceptives work.