Thyroid Hormones, Hyperthyroidism, Hypothyroidism, Symptoms, Treatment and Brand Generic Drugs
Table of Contents
Thyroid Gland
The thyroid is a butterfly-shaped endocrine gland located in the anterior neck (below the larynx, spanning the trachea). It produces hormones that regulate:
- Metabolism (energy use)
- Growth & development
- Body temperature
- Heart & nervous system function
Thyroid Hormone
There are three main types of thyroid hormones, but two of them are the most biologically important. Here’s a breakdown:
1. Classic Thyroid Hormones (Regulate Metabolism)
| Hormone | Full Name | Key Features |
| T4 | Thyroxine (Tetraidothyronine) | – Major secreted hormone (90%) – Prohormone: Converted to T3 in tissues – Long half-life (~7 days) |
| T3 | Triiodothyronine | – Biologically active form (3–4x more potent than T4) – Only 10% secreted directly; rest comes from T4 conversion – Short half-life (~1 day) |
2. Additional Thyroid Hormone (Calcium Regulation)
| Hormone | Full Name | Key Features |
| Calcitonin | – | – Produced by C-cells (parafollicular cells) in thyroid – Lowers blood calcium (inhibits osteoclasts) – Minor role compared to PTH (parathyroid hormone) |
1. T4 – Thyroxine
- Most abundant thyroid hormone (~90%)
- Inactive form, acts as a storage hormone
- Converted to T3 in the body’s tissues
- Function: Precursor to T3; maintains steady levels
2. T3 – Triiodothyronine
- Active form of thyroid hormone
- More potent than T4 (3–5x stronger)
- Only about 10% made by thyroid, most is converted from T4
- Function: Controls metabolism, heart rate, body temperature, brain function, and more
3. Calcitonin
- Produced by the C cells (parafollicular cells) of the thyroid
- Unrelated to T3/T4, but still a thyroid hormone
- Function: Lowers blood calcium levels (minor role in calcium balance compared to parathyroid hormone)
Easy Comparison
| Hormone | Full Name | Role | Activity |
| T4 | Thyroxine | Storage hormone | Inactive |
| T3 | Triiodothyronine | Main active form | Active |
| Calcitonin | — | Lowers calcium | Active (minor role) |
Hormone Production Pathway
Hypothalamus → TRH → Pituitary → TSH → Thyroid → T3 and T4
TRH (Thyrotropin-Releasing Hormone) – from hypothalamus
TSH (Thyroid-Stimulating Hormone) – from pituitary
T3/T4 – from thyroid gland
TRH (Thyrotropin-Releasing Hormone) – from hypothalamus
TSH (Thyroid-Stimulating Hormone) – from pituitary
T3/T4 – from thyroid gland
Hypothalamus
TRH (Thyrotropin-releasing hormone)
→
Pituitary
TSH (Thyroid-stimulating hormone)
→
Thyroid
T3 and T4
Click each step to view more details about each process.
Step-by-Step Explanation of the Thyroid Hormone Regulation Pathway:
Hypothalamus (in the brain):
This part of your brain acts like a command center. It monitors your body’s needs and starts the process when more thyroid hormones are required.- 👉 Hypothalamus releases a hormone called TRH (Thyrotropin-Releasing Hormone).
TRH travels to the Pituitary Gland (also in the brain):
The pituitary gland is like a messenger station that gets signals from the hypothalamus and then tells other glands what to do.- 👉 In response to TRH, the pituitary gland releases TSH (Thyroid-Stimulating Hormone).
TSH travels through the blood to the Thyroid Gland (in your neck):
Now the message reaches the thyroid gland, telling it to make and release thyroid hormones.- 👉 The thyroid responds by producing T4 (thyroxine) and a smaller amount of T3 (triiodothyronine).
T4 is converted to T3 in tissues:
T4 is the storage or inactive form. In various body tissues (like the liver and kidneys), it’s converted to T3, which is the active form that controls metabolism and energy use.Your body now has the right amount of T3 and T4 circulating to regulate important functions like:
- Metabolism
- Heart rate
- Temperature
- Energy levels
- Growth and development
Functions of Thyroid Hormones:
- Metabolic rate – ↑ Basal metabolic rate (BMR)
- Thermogenesis – Maintains body temperature
- Growth & development – Essential for brain development in infants
- Cardiovascular – ↑ Heart rate and cardiac output
- GI function – ↑ Motility
- Lipid and glucose metabolism – Enhances lipolysis, glycogenolysis
- Mood and cognition – Affects mental status and energy levels
Role of TSH (Thyroid-Stimulating Hormone)
TSH (Thyroid-Stimulating Hormone), also called thyrotropin, is a pituitary hormone that regulates thyroid function. It is the key controller of thyroid hormone production and release.
1. Primary Functions of TSH
A. Stimulates Thyroid Hormone Production
- Triggers T4/T3 Synthesis: TSH binds to receptors on thyroid follicular cells, activating:
- Iodine uptake (via sodium-iodide symporter, NIS).
- Thyroglobulin (Tg) production.
- Enzymes for T4/T3 formation (thyroid peroxidase, TPO).
B. Promotes Thyroid Growth
- Chronic TSH stimulation → thyroid enlargement (goiter).
C. Maintains Feedback Balance
- Low T4/T3 → TSH rises (signals thyroid to work harder).
- High T4/T3 → TSH falls (prevents overproduction).
2. Clinical Significance of TSH
A. Diagnostic Marker
- First-line test for thyroid disorders:
- High TSH = Hypothyroidism (underactive thyroid).
- Low TSH = Hyperthyroidism (overactive thyroid).
- B. Guides Treatment
- Hypothyroidism: Goal is to normalize TSH with levothyroxine (T4).
- Hyperthyroidism: Goal is to suppress TSH (with antithyroid drugs/surgery).
HYPERTHYROIDISM
(“Hyper” = too much)
What is Hyperthyroidism?
A condition where the thyroid gland produces too much T3 and T4 hormones, leading to an overactive metabolism.Hyperthyroidism Causes:
- Graves’ Disease – autoimmune (most common cause)
- Toxic multinodular goiter
- Thyroid adenoma (benign tumor)
- Thyroiditis (inflammation)
- Excess iodine intake or overuse of thyroid meds
Symptoms of Hyperthyroidism:
- Metabolism: Weight loss despite increased appetite
- Cardiovascular: Fast heart rate (tachycardia), palpitations
- Nervous: Anxiety, restlessness, irritability, tremors
- Skin: Warm, moist skin, sweating, hair thinning
- GI: Frequent bowel movements, diarrhea
- Eyes: Bulging eyes (exophthalmos) in Graves’ disease
- Menstrual: Irregular or lighter periods
- Others: Heat intolerance, insomnia, fatigue
HYPORTHYROIDISM
(“Hypo” = too little)
What is Hypothyroidism?
A condition where the thyroid gland doesn’t produce enough T3 and T4, causing a slowed metabolism.Causes of Hypothyroidism:
- Hashimoto’s Thyroiditis – autoimmune (most common)
- Iodine deficiency
- Thyroid surgery or radiation
- Medications (e.g., lithium, amiodarone)
- Congenital hypothyroidism
Symptoms of Hypothyroidism:
- Metabolism: Weight gain despite poor appetite
- Cardiovascular: Slow heart rate (bradycardia)
- Nervous: Depression, fatigue, poor memory
- Skin: Dry, coarse skin, cold intolerance
- GI: Constipation
- Hair: Hair thinning or hair loss, brittle nails
- Menstrual: Heavy or irregular periods
- Others: Puffy face, hoarseness, low energy, slow reflexes
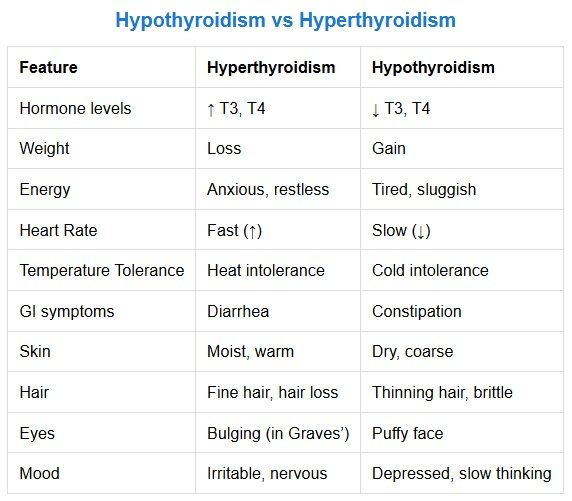
Hypothyroidism vs Hyperthyroidism
| Feature | Hyperthyroidism | Hypothyroidism |
| Hormone levels | ↑ T3, T4 | ↓ T3, T4 |
| Weight | Loss | Gain |
| Energy | Anxious, restless | Tired, sluggish |
| Heart Rate | Fast (↑) | Slow (↓) |
| Temperature Tolerance | Heat intolerance | Cold intolerance |
| GI symptoms | Diarrhea | Constipation |
| Skin | Moist, warm | Dry, coarse |
| Hair | Fine hair, hair loss | Thinning hair, brittle |
| Eyes | Bulging (in Graves’) | Puffy face |
| Mood | Irritable, nervous | Depressed, slow thinking |
Mnemonics for Thyroid Symptoms
Mnemonics for Hypothyroidism (Underactive Thyroid) – “SLOWED”
- S – Sluggish (fatigue, lethargy)
- L – Low heart rate (bradycardia)
- O – Overweight (weight gain)
- W – Weakness (muscle aches)
- E – Edema (puffy face, myxedema)
- D – Depression & Dry skin
Mnemonics for Hyperthyroidism (Overactive Thyroid) – “FAST”
- F – Feverish (heat intolerance)
- A – Anxious (nervousness, irritability)
- S – Sweating & Skin thinning
- T – Tachycardia (rapid heart rate) & Tremors
Bonus Contrast Mnemonic:
- Hypothyroidism = “Everything is SLOW” (cold, tired, constipated, gaining weight).
- Hyperthyroidism = “Everything is FAST” (hot, anxious, diarrhea, losing weight).
Thyroid Test & Lab Values
Thyroid tests measure hormone levels to diagnose hypothyroidism, hyperthyroidism, and other thyroid disorders. Here’s a breakdown of key tests, their normal ranges, and interpretations.
1. Primary Thyroid Hormones
| Test | Normal Range | Hyperthyroidism | Hypothyroidism | What It Measures |
| TSH (Thyroid-Stimulating Hormone) | 0.4–4.0 mIU/L | ↓ Low (<0.1) | ↑ High (>10) | Pituitary hormone that regulates T4/T3 production |
| Free T4 (Thyroxine) | 0.8–1.8 ng/dL | ↑ High (>1.8) | ↓ Low (<0.8) | Active form of thyroxine (major thyroid hormone) |
| Free T3 (Triiodothyronine) | 2.3–4.2 pg/mL | ↑ High (>4.2) | Normal or ↓ Low | More potent but short-lived thyroid hormone |
- Hyperthyroidism: Low TSH + High T4/T3
- Hypothyroidism: High TSH + Low T4
Why Free T4 & Free T3?
- “Free” = Bioavailable (not protein-bound).
- More accurate than Total T4/T3 (affected by pregnancy, medications, liver disease).
2. Thyroid Antibodies (Autoimmune Testing)
| Test | Significance |
| TPO Antibodies (Thyroid Peroxidase) | Elevated in Hashimoto’s thyroiditis (hypothyroidism) |
| TRAb (TSH Receptor Antibodies) | Elevated in Graves’ disease (hyperthyroidism) |
| Thyroglobulin Antibodies | Seen in Hashimoto’s or thyroid cancer monitoring |
Interpreting Thyroid Lab Results
A. Hypothyroidism (Underactive Thyroid)
Primary Hypothyroidism (Most Common):
- ↑ TSH (High)
- ↓ Free T4 (Low)
- Cause: Hashimoto’s (check TPO antibodies), iodine deficiency, thyroid surgery.
Secondary Hypothyroidism (Rare – Pituitary Issue):
- ↓ or Normal TSH
- ↓ Free T4
B. Hyperthyroidism (Overactive Thyroid)
Primary Hyperthyroidism:
- ↓ TSH (Low or Suppressed)
- ↑ Free T4 and/or Free T3
- Cause: Graves’ disease (check TRAb), toxic nodules, thyroiditis.
Subclinical Hyperthyroidism:
- ↓ TSH (Low)
- Normal Free T4 & T3
C. Euthyroid Sick Syndrome (Non-Thyroidal Illness)
- Low T3, Normal/Low T4, Normal/High TSH
- Seen in critically ill patients (not a true thyroid disorder).
Thyroid Lab Interpretation Table
| Condition | TSH | Free T4 | Free T3 | Antibodies |
| Primary Hypo | ↑↑ | ↓ | Normal/↓ | TPO (+) |
| Primary Hyper | ↓↓ | ↑ | ↑ | TRAb (+) (Graves’) |
| Subclinical Hypo | ↑ | Normal | Normal | – |
| Subclinical Hyper | ↓ | Normal | Normal | – |
| Thyroiditis | Varies | Varies | Varies | TPO/TRAb (+) |
Thyroid Medications (Treatment)
| Brand Name | Generic Name | Mechanism of Action | Used For | Important points |
| Synthroid, Levoxyl, Euthyrox, Unithroid | Levothyroxine sodium | Synthetic T4; converts to T3 in the body to regulate metabolism | Hypothyroidism |
|
| Cytomel | Liothyronine sodium | Synthetic T3; directly active thyroid hormone | Hypothyroidism |
|
| Armour Thyroid, NP Thyroid, Nature-Throid | Desiccated thyroid (USP) | Natural T4 & T3 combination from porcine thyroid glands | Hypothyroidism |
|
| Tapazole | Methimazole | Inhibits thyroid peroxidase enzyme; blocks T4/T3 synthesis | Hyperthyroidism |
|
| (No brand; generic only) | Propylthiouracil (PTU) | Inhibits T4/T3 synthesis and blocks peripheral conversion of T4 to T3 | Hyperthyroidism (esp. in pregnancy) |
|
| (No brand; radioactive isotope) | Radioactive Iodine (I-131) | Destroys overactive thyroid tissue via radiation (may cause permanent hypothyroidism). | Hyperthyroidism, Thyroid Cancer Graves’ disease, toxic nodules. | Post-Treatment: Monitor TSH, start levothyroxine if needed. |
| No Brand | Potassium Iodide (Lugol’s Solution, SSKI) | High iodine inhibits thyroid hormone synthesis and release Shrinks the thyroid gland and reduces blood flow. Rapid reduction in T4/T3 levels. | Thyroid storm, pre-surgery (shrinks thyroid). |
|
| Inderal | Propranolol | Non-selective beta-blocker; reduces symptoms like tremors, palpitations | Symptom control in hyperthyroidism | Controls symptoms Controls tachycardia, tremors, anxiety. |
| Tenormin | Atenolol | Beta-1 selective blocker; reduces heart rate and tremors | Symptom control in hyperthyroidism | Symptoms management Tachycardia (↓ heart rate), Palpitations, Tremors, Anxiety |
Synthetic vs. Natural Thyroid Medications
Synthetic Thyroid Medications
(e.g., Levothyroxine/Synthroid, Liothyronine/Cytomel) Pros:- Consistent potency: Precise dosing (FDA-regulated).
- T4-only (Levothyroxine): Mimics natural thyroid hormone conversion (T4→T3).
- Guideline-recommended: First-line for hypothyroidism (AACE/ATA).
- Fewer side effects: No risk of excess T3 (unlike natural desiccated thyroid).
❌ Some patients report persistent symptoms (fatigue, brain fog) despite “normal” TSH.
❌ Requires peripheral conversion (T4→T3), which may be inefficient in some patients.
Why Patients Might Prefer Synthetic:
- Trust in evidence-based medicine.
- Prefer stability and predictability of lab-made hormones.
Natural Desiccated Thyroid (NDT)
(e.g., Armour Thyroid, NP Thyroid) Pros:- Contains both T4 + T3: May benefit patients with conversion issues.
- Historical use: Used for decades before synthetic options.
- Some patients report better symptom relief (energy, mood, weight).
❌ Variable potency: Batch-to-batch differences (less regulated).
❌ Risk of excess T3: Can cause palpitations, anxiety, or bone loss.
❌ Not guideline-preferred: Limited evidence of superiority over levothyroxine.
Why Patients Might Prefer NDT:
- Belief in “natural” therapies.
- Frustration with ongoing symptoms on levothyroxine.
- Anecdotal reports of improved well-being.
Why Some Patients Switch from Synthetic to Natural Thyroid Meds:
- Persistent Symptoms
- Despite “normal” TSH, some patients feel better on NDT (possibly due to T3 content).
- Conversion Issues
- Genetic variations (e.g., DIO2 gene) may impair T4→T3 conversion.
- Distrust of Synthetic Drugs
- Preference for “whole gland” therapy.
Why Doctors Often Prefer Synthetic Thyroid Meds:
- Predictable Dosing
- NDT’s T4:T3 ratio (4:1) doesn’t match human thyroid secretion (~14:1).
- Safety Concerns
- Excess T3 in NDT may cause cardiac strain or osteoporosis.
- Lack of Strong Evidence
- Most studies show no significant difference in outcomes vs. levothyroxine.
Who Might Benefit from Natural Thyroid?
- Patients with documented T4→T3 conversion issues.
- Those who fail levothyroxine monotherapy despite dose optimization.
- Individuals who philosophically prefer natural treatments (after informed discussion).
Who Should Stick with Synthetic?
Newly diagnosed hypothyroidism (first-line).
- Pregnant women (requires precise TSH control).
- Cardiac patients (T3 in NDT can stress the heart).
Medical conditions & their treatments with thyroid medications
1. Hypothyroidism (Underactive Thyroid)
- Causes: Hashimoto’s, thyroidectomy, iodine deficiency. Treatment:
- First-line: Levothyroxine (Synthroid) – Replaces T4.
- Dose: 1.6 mcg/kg/day (start low in elderly/cardiac patients).
- Monitor: TSH every 6–8 weeks.
- Liothyronine (Cytomel) – T3 replacement (rarely used alone).
- Desiccated thyroid (Armour) – T4 + T3 combo (not guideline-preferred).
- Take levothyroxine first thing in the morning on an empty stomach with plain water.
- Do not eat or drink anything for at least 1.5 hrs before or after the medication.
- Avoid calcium/iron supplements within 4 hours.
2. Hyperthyroidism (Overactive Thyroid)
- Causes: Graves’ disease, toxic nodules, thyroiditis. Treatment:
- First-line: Methimazole (Tapazole) – Blocks thyroid hormone synthesis.
- Dose: 5–30 mg/day (taper to maintenance).
- Avoid in 1st trimester pregnancy (use PTU instead).
- Use: Thyroid storm, 1st-trimester pregnancy.
- Monitor Free T4/T3 (TSH may lag).
- Methimazole side effects: Agranulocytosis (check CBC if fever/sore throat).
3. Thyroid Storm (Life-Threatening Hyperthyroidism)
Treatment:- PTU (preferred over methimazole) – 200–300 mg every 6h.
- Beta-blockers (Propranolol) – Controls heart rate.
- Lugol’s solution/SSKI – Blocks hormone release (give after PTU).
- Steroids (Hydrocortisone) – Inhibits T4→T3 conversion.
- ICU admission required.
- Avoid aspirin (risks T3 release).
4. Post-Thyroidectomy Management
For Cancer:- Levothyroxine at suppressive doses (TSH <0.1 mIU/L). For Benign Disease:
- Levothyroxine replacement (goal TSH: 0.5–2.5 mIU/L).
- Check calcium post-op (risk of hypoparathyroidism).
5. Subclinical Hypothyroidism (TSH ↑, Normal T4)
Treatment:- Treat if TSH >10 or symptomatic (fatigue, weight gain).
- Levothyroxine (start 25–50 mcg/day).
- Recheck TSH in 6–8 weeks.
6. Pregnancy & Thyroid Disorders
Hypothyroidism:
- Increase levothyroxine dose by 25–30% (TSH goal: <2.5 mIU/L).
Hyperthyroidism:
- 1st trimester: PTU.
- 2nd/3rd trimester: Switch to methimazole.
- Monitor TSH every 4 weeks.
7. Myxedema Coma (Severe Hypothyroidism)
Treatment:- IV Levothyroxine (300–500 mcg loading dose).
- Liothyronine (T3) if critical (due to peripheral conversion impairment).
- Glucocorticoids (for adrenal insufficiency risk).
- Slow rewarming, avoid sedatives.
8. Thyroid Cancer (Post-Thyroidectomy)
Treatment:- Levothyroxine suppression therapy (TSH <0.1 mIU/L for high-risk cancer).
- Radioactive iodine (I-131) – For residual/metastatic disease.
Some common terms associated with Thyroid Medical Conditions
Thyroid Eye Disease (TED)
- An autoimmune condition, often linked with Graves’ disease, where immune cells attack the tissues around the eyes.
- Symptoms: Bulging eyes, dryness, redness, eye pain, double vision, swelling.
Thyroid Knot
- Typically refers to a thyroid nodule—a lump or abnormal growth in the thyroid.
- Can be benign or cancerous.
- May cause visible swelling or be found incidentally.
Thyroid Storm
- A rare, life-threatening complication of untreated or poorly managed hyperthyroidism.
- Symptoms: High fever, rapid heart rate, agitation, delirium, vomiting, coma.
- Requires emergency treatment.
Thyroiditis
- Inflammation of the thyroid gland.
- Types: Hashimoto’s (chronic), De Quervain’s (painful), postpartum, silent.
- Can lead to hypothyroidism or hyperthyroidism, depending on the stage.
Thyrotoxicosis
- A state of excess thyroid hormones in the body.
- Can result from hyperthyroidism, thyroiditis, or excess hormone intake.
- Symptoms: Weight loss, heat intolerance, tremors, palpitations, anxiety.
Thyroid Eye Disease Symptoms
- Bulging/protruding eyes
- Dry or watery eyes
- Light sensitivity
- Double vision
- Eye pressure or pain
- Eyelid retraction
Thyroid Goiter
- An enlargement of the thyroid gland.
- May occur with normal, low, or high thyroid hormone levels.
- Can cause a visible neck swelling or pressure symptoms.
Thyroid Hair Loss
- Common with both hypothyroidism and hyperthyroidism.
- Hair becomes dry, brittle, and falls out easily.
- Usually reversible with proper thyroid treatment.
Thyroid Belly
- Refers to weight gain or bloating often associated with hypothyroidism.
- Slowed metabolism leads to fat accumulation, especially around the abdomen.
Thyroid Rash
- Rashes can occur with:
- Autoimmune thyroid disease (e.g., Hashimoto’s, Graves’)
- Medication side effects (e.g., methimazole allergy)
- Skin changes from hormonal imbalances
Thyroid Cyst
- A fluid-filled sac in the thyroid gland.
- Usually benign and asymptomatic.
- Large cysts may cause neck discomfort or swallowing issues.
Thyroid Bulging Eyes
- Another name for exophthalmos, a hallmark of Graves’ disease / Thyroid Eye Disease.
- Caused by inflammation and swelling in eye muscles and tissues behind the eyes.
Frequently asked Questions and Answers
What are the Best Foods for Thyroid Patients
For Hypothyroidism:
- Fruits: Berries, apples, peaches, pears, grapes, citrus fruits, pineapple, bananas. Healthline
- Non-starchy Vegetables: Greens, artichokes, zucchini, asparagus, carrots, peppers, spinach, mushrooms. Healthline
- Starchy Vegetables: Sweet potatoes, potatoes, peas, butternut squash. Healthline
- Lean Proteins: Fish, shellfish, eggs, turkey, chicken. Healthline
- Healthy Fats: Olive oil, avocados, coconut oil, full-fat yogurt. Healthline
For Hyperthyroidism:
- Foods rich in selenium (e.g., Brazil nuts), iron (e.g., leafy greens), calcium, and vitamin D may be beneficial.
What Foods to Avoid with Thyroid Conditions
Hypothyroidism:
- Fried fast foods, processed foods high in salt, sugary treats (pastries, cakes, cookies, ice cream), excessive alcohol.
Hyperthyroidism:
- High-iodine foods, soy products, gluten, caffeine. Medical News Today
Best Cream for Thyroid-Related Dry Skin
For very dry skin, thicker moisturizers or oils are recommended. Products containing ammonium lactate or urea can help dissolve dead skin and allow moisturizers to penetrate more effectively.Does Biotin Affect the Thyroid?
Biotin does not affect thyroid hormone levels or thyroid function. However, high doses can interfere with laboratory tests, leading to inaccurate thyroid function results. It’s advisable to stop taking biotin at least two days before thyroid testing. SourceCauses of Thyroid Disease in Females
- Autoimmune Diseases: Conditions like Hashimoto’s thyroiditis and Graves’ disease are more prevalent in women and can lead to hypothyroidism or hyperthyroidism.
- Hormonal Changes: Pregnancy, menopause, and other hormonal fluctuations can increase the risk.
- Iodine Deficiency: Essential for thyroid hormone production; deficiency can lead to hypothyroidism. Cleveland Clinic
What are the causes of thyroid cancer?
- Genetic mutations
- Radiation exposure (especially in childhood)
- Family history of thyroid or other endocrine cancers
- Iodine deficiency (linked to some types)
- Certain inherited conditions like MEN syndrome
What are the causes of overactive thyroid (Hyperthyroidism)?
- Graves’ disease (most common cause)
- Thyroid nodules (toxic adenoma or multinodular goiter)
- Thyroiditis (temporary release of stored hormones)
- Excessive iodine intake
- Overmedication with thyroid hormone
Does thyroid affect periods?
Yes.- Hypothyroidism: May cause heavy, irregular, or prolonged periods.
- Hyperthyroidism: May cause light, infrequent, or missed periods.
Does thyroid affect blood pressure?
Yes.- Hypothyroidism: Can lead to high diastolic BP (bottom number).
- Hyperthyroidism: May cause high systolic BP (top number), rapid heartbeat.
Is thyroid treatable?
Yes.- Most thyroid conditions (hypo-, hyperthyroidism, nodules, goiters) are treatable with medications, radioactive iodine, or surgery.
- Even thyroid cancer, especially papillary type, is often highly treatable.
Does thyroid affect pregnancy?
Yes.- Untreated thyroid disorders can cause infertility, miscarriage, premature birth, and developmental issues in the baby.
- Proper management is important before and during pregnancy.
Is thyroid a hereditary disease?
Partially, yes.- Conditions like Graves’ disease, Hashimoto’s, and some thyroid cancers can run in families.
- A family history increases the risk but doesn’t guarantee disease.